In October 2021, the American Academy of Pediatrics, alongside the Academy of Child and Adolescent Psychiatry and the Children’s Hospital Association, declared a national emergency in children’s mental health – citing the stress brought on by the COVID-19 pandemic and the ongoing fight for racial justice as key factors in the worsening mental health crisis.
These challenges have affected children across the board, and those in rural areas have been particularly affected. Given this population’s proximity to mental health resources and other unique barriers like transportation and economic hardship, getting behavioral health support isn’t always possible.
Thankfully, with the right solutions at play, healthcare organizations can help the youth in their communities access the right help at the right time – regardless of geographical barriers.
Common mental health challenges rural youth face
One of the first steps to helping rural youth is understanding their experiences. Rural communities face increased economic hardships and have fewer community resources available. Whether it’s medical or behavioral health care, there is a lack of options for individuals in rural communities.
Let’s take a closer look at a few of these barriers rural youth may face when seeking mental health care:
Less access to care: When fewer services are available, there’s a lack of opportunities for children to get help. If a child needs specialty care, their family may need to travel long distances. A commute to see a specialist may require time away from work and school – which may not be feasible for ongoing care.
Substance use challenges: Rural areas have experienced an uptick in substance use rates for youth and adults alike. When it comes to addressing these challenges in kids, it can be difficult to find the correct treatment. Additionally, caregivers who struggle with substance use may be unable to provide consistent care and support.
Mental health stigma: Stigma can prove even more challenging for those living in rural communities with limited access to mental health resources. This population deals with unique barriers regarding anonymity in their communities, health literacy, pervasive provider shortages, transportation challenges, and religious barriers.
While these challenges might feel daunting, there are several best practices that can help create increased opportunities for mental health care.
The role of telepsychiatry in rural America
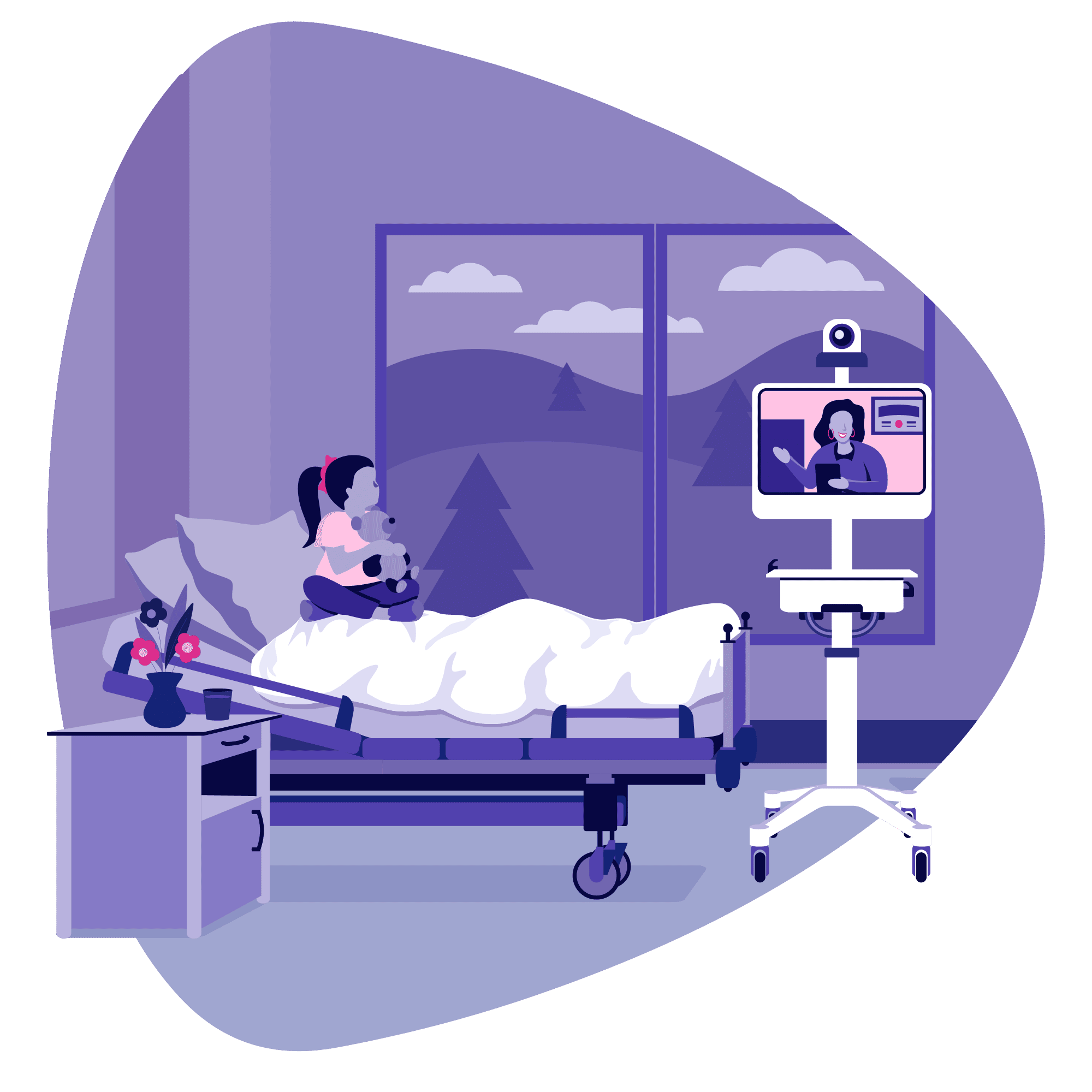
Gaining access to specialty providers can prove challenging for healthcare organizations in rural America. However, that’s what makes telepsychiatry an essential best practice for reaching youth in these communities. Telepsychiatry connects organizations with a large pool of providers from all over the U.S. to help ensure they have the right behavioral health specialist to meet the needs of their communities. At Iris Telehealth, we call this process provider matching.
This approach helps organizations find the perfect provider fit to address their communities’ challenges effectively. Additionally, telepsychiatry allows children to connect to high-quality, specialty providers from the privacy of their homes. Virtual access to behavioral health care also enables this population to get help and maintain their anonymity at a community level.
The American Psychiatric Association (APA) calls telepsychiatry’s reach into rural and remote areas one of the best successes of telemedicine. The APA also cites that satisfaction has been superior for patients, families, and providers.
How healthcare organizations can support their communities
Reaching this community with high-quality care starts with implementing some best practices. Here are a few ideas your organization may consider to help support the mental health needs of your community:
Create a centralized location for care: When it comes to virtual care, ensuring patients have internet access is essential. For healthcare organizations in rural communities, that might look like creating a centralized place where patients can go for their appointments. In most clinical settings, a medical assistant will bring the patient into the room to ensure everything is ready to go for the appointment. This provider will confirm an internet connection and introduce the patient to the doctor.
Set expectations: When using telepsychiatry, setting expectations upfront is essential. This process may start with educating the patients about what they can expect during a telepsychiatry visit. For patients accessing their telehealth appointment from home, providers should let them know that all the rules for a confidential in-person health appointment apply to telepsychiatry. Providers can also check in with the patients and families about how they’re feeling about telehealth, ask what’s working, and let them know that it might take time to adjust to the platform.
Educate the community: Healthcare organizations can reach more kids by communicating with schools about what behavioral health support is available. This approach also connects healthcare organizations with school counselors who can make referrals.
Provide family support: The COVID-19 pandemic has been a prolonged trauma. Research from previous disasters and traumas show that a child’s ability to handle stress is directly related to their caregiver’s ability to handle anxiety. So, making sure that the child’s caregiver has support is a central component in helping a child’s mental health.
Amid a behavioral health crisis, there’s always a need for education around anxiety related to going back to school, the COVID-19 pandemic, gun violence, and anything else that may occur in the community. Thankfully, there are always outreach opportunities to educate families, provide support, and increase awareness of available community resources.
Where Iris Telehealth fits in
At Iris, we partner with communities in need of mental health resources. By providing rural populations access to specialty behavioral health providers from around the country, we can help support their needs. Contact us today if you would like to learn more about how telepsychiatry can support your community.